|
Getting your Trinity Audio player ready...
|
Cataracts are one of the most common causes of vision impairment, especially in older adults. They occur when the lens of the eye becomes cloudy, leading to blurry vision. Cataract surgery is a highly effective way to restore vision, and there are several types of cataract surgery available today. In this blog, we will explore what are the 3 types of cataract surgery, how they work, and which type might be right for you.
What is Cataract Surgery?
Cataract surgery is a medical procedure in which the cloudy lens of the eye (the cataract) is removed and replaced with an artificial lens. This surgery is typically performed under local anesthesia and does not require a hospital stay. Cataract surgery has a high success rate and can significantly improve vision, often restoring clear sight within a few days of recovery.
What Are the 3 Types of Cataract Surgery?
There are three main types of cataract surgery that are commonly performed: Phacoemulsification, Extracapsular Cataract Extraction, and Intracapsular Cataract Extraction. Each of these surgeries has its advantages and may be selected based on the patient’s specific condition and the severity of the cataract.
Let’s take a closer look at each of these types:
1. Phacoemulsification (Small Incision Cataract Surgery)
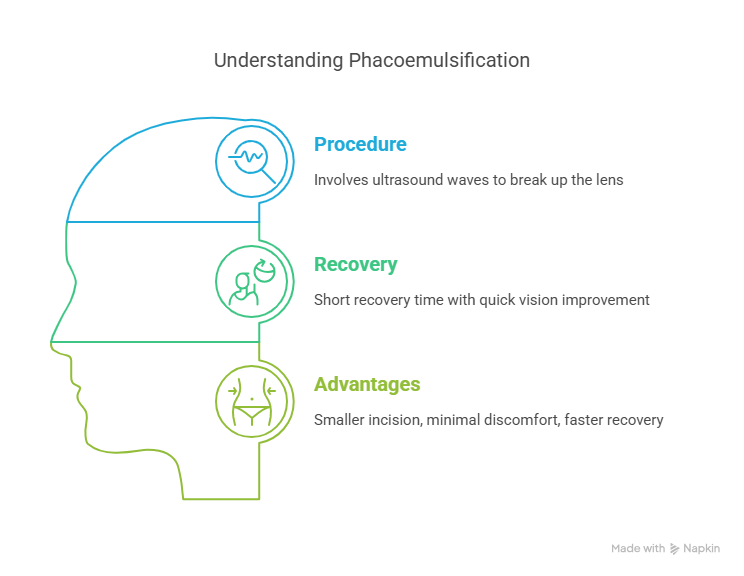
Phacoemulsification is the most commonly performed cataract surgery today. It is a minimally invasive procedure that involves the use of ultrasound waves to break up the cloudy lens into small fragments, which are then suctioned out of the eye. After the cataract is removed, an artificial intraocular lens (IOL) is implanted to replace the cloudy lens and restore clear vision.
- How It Works: During phacoemulsification, the surgeon makes a small incision in the cornea (the clear front part of the eye). A probe is then inserted into the eye, which emits high-frequency sound waves to break the cataract into smaller pieces. These pieces are suctioned out through the same small incision.
- Recovery: The recovery time for phacoemulsification is relatively short, with most patients experiencing improved vision within a few days. The small incision typically heals on its own without the need for stitches.
- Advantages: The key benefits of phacoemulsification are that it involves a smaller incision, minimal discomfort, and a faster recovery time. This type of surgery is ideal for people with age-related cataracts and is effective in removing cataracts at different stages of development.
2. Extracapsular Cataract Extraction (ECCE)
Extracapsular Cataract Extraction is a more traditional method of cataract surgery. This type of surgery is generally recommended for more advanced cataracts that are too hard or large to be treated by phacoemulsification. In ECCE, the cloudy lens is removed in one piece, and an artificial intraocular lens is placed inside the eye.
- How It Works: In ECCE, the surgeon makes a larger incision in the eye, usually between 10 and 12 millimeters, to remove the cataract. The lens is removed in one large piece, and the remaining capsule is left intact to hold the new IOL. The artificial lens is then inserted into the eye to replace the cloudy lens.
- Recovery: The recovery from ECCE takes longer than phacoemulsification. Patients may need to rest their eyes for a few days to several weeks and may require post-operative care, including the use of eye drops to prevent infection and reduce inflammation.
- Advantages: ECCE is often recommended when the cataract is too hard or advanced for phacoemulsification. It is highly effective for restoring vision in cases where phacoemulsification cannot be performed. However, it requires a larger incision and a longer recovery period compared to phacoemulsification.
3. Intracapsular Cataract Extraction (ICCE)
Intracapsular Cataract Extraction is the least commonly performed type of cataract surgery. It is typically reserved for very rare and complex cases where the cataract has caused severe complications, such as when the cataract has become dislocated or when the patient has other eye conditions like glaucoma or retinal diseases.
- How It Works: In ICCE, the entire lens, including the capsule that holds the lens in place, is removed. The incision required for ICCE is larger than the other two types of cataract surgery. After the cataract and capsule are removed, the eye is examined, and the surgeon may insert an IOL or a different type of lens implant.
- Recovery: The recovery from ICCE can be more difficult than the other two types of surgery. The patient may need to wear an eye patch for several days and use prescribed medications to help with the healing process. Full recovery may take several weeks or longer.
- Advantages: ICCE is effective in extremely difficult cataract cases and can offer good results, but the procedure is more invasive and carries more risks. As a result, it is rarely used today and is usually reserved for only the most severe or complicated cataract cases.
Which Type of Cataract Surgery is Right for You?
The choice of which type of cataract surgery is best for you will depend on several factors, including:
- The severity of the cataract: If the cataract is small or moderately advanced, phacoemulsification is often the best option. For larger or harder cataracts, ECCE may be needed.
- Your overall eye health: If you have other eye conditions such as glaucoma or diabetic retinopathy, ICCE may be considered in certain situations. However, in most cases, the surgeon will aim for less invasive methods if possible.
- Your age and general health: Younger patients may be more likely to have phacoemulsification as their option, while older patients with more advanced cataracts may need ECCE or ICCE.
- Your surgeon’s recommendation: The expertise and recommendation of your ophthalmologist will be crucial in determining which type of surgery is best suited for you. Your surgeon will evaluate your cataract’s severity, your eye health, and other factors before making a recommendation.
What Are the Risks and Complications of Cataract Surgery?
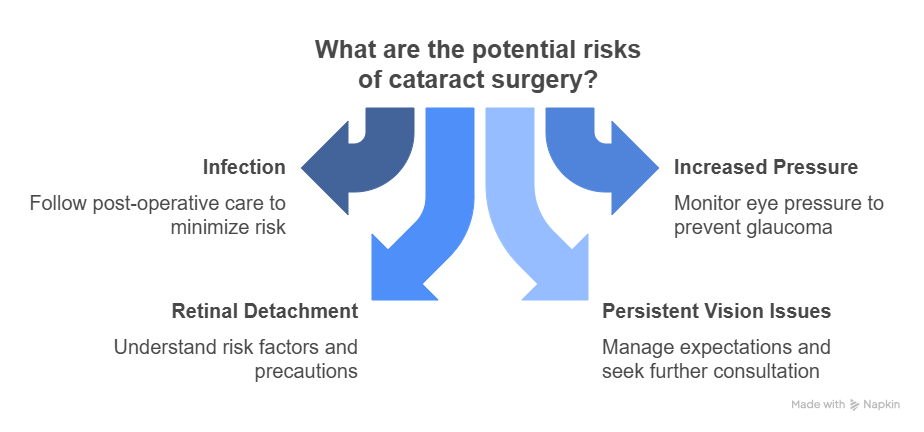
While cataract surgery is generally safe and effective, all surgeries come with potential risks. Some possible complications include:
- Infection: Though rare, infection can occur after surgery. It is important to follow your surgeon’s post-operative care instructions to reduce this risk.
- Increased intraocular pressure: Sometimes, cataract surgery can cause an increase in pressure within the eye, which can lead to glaucoma.
- Retinal detachment: This is a rare but serious complication that can occur after cataract surgery, especially in patients who are at higher risk.
- Persistent vision issues: Some patients may continue to experience blurry vision or other visual disturbances even after surgery.
Your ophthalmologist will discuss the risks and help you understand what to expect during the recovery process.
Which Cataract Surgery Is Right for You? Explore the 3 Options!
Make An AppointmentConclusion
Cataract surgery has a high success rate and can significantly improve the quality of life for people affected by cataracts. If you are experiencing blurred vision, difficulty seeing at night, or other symptoms of cataracts, it is important to consult with an experienced eye doctor. They will evaluate your condition and discuss what are the 3 types of cataract surgery to determine the best approach for you.
At IGEHRC, we offer expert care for cataract patients, providing personalized treatment options and guidance throughout the process. Whether you’re considering phacoemulsification, ECCE, or ICCE, our team will work with you to ensure the best possible outcome for your vision. If you have cataracts or are experiencing any of the symptoms, contact us today to schedule a consultation and take the first step toward clearer vision.