|
Getting your Trinity Audio player ready...
|
Few things can be as unsettling as experiencing pain in your eyes. Our eyes are not just instruments of sight; they are incredibly delicate organs, constantly working to interpret the world around us. So, when they send us a signal of discomfort, it naturally commands our attention, often bringing a sense of worry.
Eye pain can range from a mild, annoying irritation to a sharp, debilitating ache. It’s a symptom that can arise from a multitude of causes, some quite benign and easily remedied, others indicating serious underlying conditions that demand immediate medical attention. Understanding the potential Eye Pain reasons options available is crucial for anyone experiencing this discomfort. Today, we’re going to explore the various reasons behind eye pain, delve into their common symptoms, and discuss the appropriate treatments, guiding you on when to simply rest and when to seek professional help. At Indira Gandhi Eye Hospitals, we believe in empowering you with knowledge, ensuring you know exactly when to act to protect your precious eyesight.
Understanding Eye Pain: A Spectrum of Discomfort
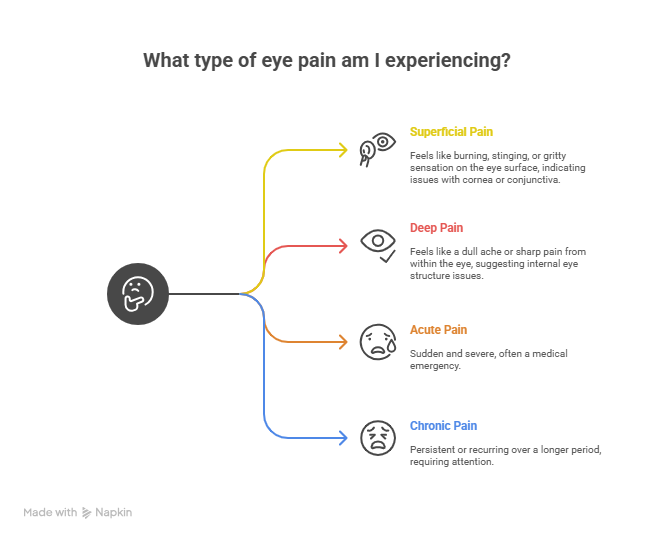
Before we dive into specific causes, it’s helpful to understand that eye pain isn’t always the same. It can manifest in different ways, offering clues to its origin:
- Superficial Pain (Ocular Surface Pain): This type of pain feels like it’s on the surface of your eye, often described as a burning, stinging, itching, or gritty sensation. It usually indicates an issue with the cornea (the clear front surface), conjunctiva (the clear membrane covering the white part of the eye and inner eyelids), or the eyelids themselves.
- Deep Pain (Orbital or Ocular Pain): This feels like a dull ache, throbbing, or sharp, piercing pain coming from within the eye or behind it. This type of pain often suggests a more serious underlying issue affecting internal eye structures, muscles around the eye, or even nerves.
- Acute vs. Chronic Pain: Acute pain is sudden and often severe, while chronic pain is persistent or recurring over a longer period. Both warrant attention, but acute, severe pain is often a medical emergency.
The presence of other symptoms alongside the pain, such as redness, discharge, sensitivity to light, blurred vision, headache, or nausea, provides vital clues to determine the Eye Pain Reason that might be needed.
Suffering from persistent eye pain? Book an appointment with our eye specialist today for accurate diagnosis and effective treatment.
Book Appointment TodayCommon Surface Eye Pain: Reasons and Treatments
Many instances of eye pain originate from issues on the surface of the eye. While often less severe than deep pain, they can still be incredibly uncomfortable and require attention.
- Foreign Body Sensation:
- Reason: Something tiny like a speck of dust, grit, sand, an eyelash, a bit of makeup, or even a dislodged contact lens gets into your eye.
- Symptoms: Sudden, sharp, scratching pain, excessive tearing, redness, and a constant feeling that “something is in my eye.”
- Treatment:
- Immediate Action: Blink repeatedly to encourage tearing and flush out the particle. Gently pull your upper eyelid over your lower eyelid to try and dislodge it. You can also try flushing your eye with clean water or saline solution. Avoid rubbing your eye, as this can scratch the cornea.
- When to See a Doctor: If the pain persists after flushing, if your vision becomes blurry, or if you suspect something is embedded in your eye (e.g., a metal shard, wood splinter). Your ophthalmologist can safely remove the foreign body and check for any corneal abrasions.
- Immediate Action: Blink repeatedly to encourage tearing and flush out the particle. Gently pull your upper eyelid over your lower eyelid to try and dislodge it. You can also try flushing your eye with clean water or saline solution. Avoid rubbing your eye, as this can scratch the cornea.
- Reason: Something tiny like a speck of dust, grit, sand, an eyelash, a bit of makeup, or even a dislodged contact lens gets into your eye.
- Conjunctivitis (Pink Eye):
- Reason: Inflammation of the conjunctiva, most commonly caused by viruses, bacteria, or allergens.
- Symptoms: Itchiness, redness (giving it the “pink eye” appearance), a gritty or burning sensation, and discharge.
- Viral: Watery, clear discharge, often associated with a cold or flu. Highly contagious.
- Bacterial: Thick, yellowish-green pus-like discharge, often causes eyelids to stick together, especially in the morning. Contagious.
- Allergic: Intense itchiness, watery discharge, often seasonal, and may be accompanied by sneezing or a runny nose. Not contagious.
- Viral: Watery, clear discharge, often associated with a cold or flu. Highly contagious.
- Treatment: The Eye Pain Reason here depends on the type:
- Viral: Mostly supportive care. Cold compresses can soothe discomfort, and artificial tears help lubricate. It usually resolves on its own in 1-3 weeks.
- Bacterial: Antibiotic eye drops or ointment prescribed by a doctor. Improvement is typically seen within a few days.
- Allergic: Antihistamine eye drops, cold compresses, and avoiding the allergen. Oral antihistamines may also help.
- Crucial: Practice excellent hand hygiene, avoid touching your eyes, and don’t share personal items to prevent spreading contagious infections.
- Viral: Mostly supportive care. Cold compresses can soothe discomfort, and artificial tears help lubricate. It usually resolves on its own in 1-3 weeks.
- Dry Eyes:
- Reason: This occurs when your eyes don’t produce enough tears, or the tears evaporate too quickly. Common causes include prolonged screen time, environmental factors (wind, dry air, air conditioning), aging, certain medications, and systemic diseases.
- Symptoms: Persistent burning, stinging, grittiness, redness, a feeling of foreign body, blurred vision that fluctuates, and sometimes paradoxically, excessive tearing (as the eye tries to compensate for underlying dryness).
- Treatment: Your Eye Pain Reason for dry eyes can be multi-faceted:
- Over-the-counter artificial tears (preservative-free if used frequently).
- Warm compresses to stimulate oil glands.
- Blinking exercises, taking screen breaks (20-20-20 rule).
- Humidifiers, increasing water intake.
- Prescription eye drops (e.g., cyclosporine, lifitegrast) to increase tear production.
- Punctal plugs to block tear drainage.
- Over-the-counter artificial tears (preservative-free if used frequently).
- Reason: This occurs when your eyes don’t produce enough tears, or the tears evaporate too quickly. Common causes include prolonged screen time, environmental factors (wind, dry air, air conditioning), aging, certain medications, and systemic diseases.
- Corneal Abrasion / Corneal Ulcer:
- Reason:
- Abrasion: A scratch on the cornea, caused by trauma (fingernail, branches, foreign body) or improper contact lens use.
- Ulcer: A more serious open sore on the cornea, often caused by infection (bacterial, fungal, viral) or prolonged contact lens misuse.
- Abrasion: A scratch on the cornea, caused by trauma (fingernail, branches, foreign body) or improper contact lens use.
- Symptoms: Severe pain (often described as agonizing, like something is constantly stuck in the eye), intense tearing, significant redness, extreme light sensitivity (photophobia), and blurred vision.
- Treatment: This is a medical emergency. Seek immediate care.
- Abrasion: Antibiotic eye drops or ointment to prevent infection, pain relief, and sometimes patching to allow healing. Most minor abrasions heal quickly.
- Ulcer: Aggressive antibiotic, antiviral, or antifungal eye drops, often prescribed hourly. Close monitoring is crucial as ulcers can lead to severe vision loss or even necessitate corneal transplant if not treated effectively.
- Abrasion: Antibiotic eye drops or ointment to prevent infection, pain relief, and sometimes patching to allow healing. Most minor abrasions heal quickly.
- Reason:
- Stye / Chalazion:
- Reason: A stye (hordeolum) is a painful, red, pus-filled lump on the eyelid, usually caused by a bacterial infection of an oil gland near the lash line. A chalazion is a non-infectious, typically painless lump that forms when an oil gland becomes completely blocked.
- Symptoms: Stye: Localized pain, tenderness, redness, swelling, often at the edge of the eyelid. Chalazion: A firm, painless lump on the eyelid, sometimes with mild swelling.
- Treatment: The Eye Pain Reason here focuses on relieving the blockage and inflammation:
- Warm Compresses: The most effective home treatment. Apply a clean, warm (not hot) compress to the affected eyelid for 10-15 minutes, 3-4 times a day. This helps the gland drain.
- Avoid Squeezing: Never try to pop a stye or chalazion, as this can worsen the infection.
- When to See a Doctor: If a stye doesn’t improve with home care in a few days, if it spreads, or if it affects your vision. A chalazion that doesn’t resolve or is large may require a doctor to drain it or inject a steroid.
- Warm Compresses: The most effective home treatment. Apply a clean, warm (not hot) compress to the affected eyelid for 10-15 minutes, 3-4 times a day. This helps the gland drain.
- Reason: A stye (hordeolum) is a painful, red, pus-filled lump on the eyelid, usually caused by a bacterial infection of an oil gland near the lash line. A chalazion is a non-infectious, typically painless lump that forms when an oil gland becomes completely blocked.
- Blepharitis:
- Reason: Chronic inflammation of the eyelids, often due to bacterial overgrowth, blocked oil glands, or skin conditions like rosacea or seborrheic dermatitis.
- Symptoms: Itchy, burning, red, swollen eyelids, crusty or greasy eyelashes (especially upon waking), gritty sensation in eyes, light sensitivity, sometimes loss of eyelashes.
- Treatment: Focuses on eyelid hygiene. Eye Pain Reason for blepharitis involves:
- Warm Compresses: To loosen crusts and open oil glands.
- Lid Scrubs: Gently cleaning the lash line with diluted baby shampoo or a special eyelid cleanser.
- Sometimes, antibiotic ointment or drops (for bacterial blepharitis) or steroid drops (for inflammation) are prescribed by an ophthalmologist.
- Reason: Chronic inflammation of the eyelids, often due to bacterial overgrowth, blocked oil glands, or skin conditions like rosacea or seborrheic dermatitis.
Suffering from persistent eye pain? Book an appointment with our eye specialist today for accurate diagnosis and effective treatment.
Book Appointment TodayCommon Internal/Deep Eye Pain: Reasons and Treatments
Pain originating from within the eye or behind it can be more concerning and often indicates a serious condition requiring urgent professional evaluation. Understanding this Eye Pain Reason is critical.
- Acute Angle-Closure Glaucoma:
- Reason: A sudden, rapid, and severe increase in the pressure inside the eye (intraocular pressure) due to a sudden blockage of the eye’s drainage angle. This is a medical emergency.
- Symptoms: Excruciating, sudden eye pain, often accompanied by severe headache, nausea, vomiting, sudden blurred vision, and seeing halos around lights. The eye is usually very red and feels hard to the touch.
- Treatment: Immediate medical attention is paramount to prevent permanent vision loss. Treatment involves quickly lowering the eye pressure with eye drops, oral medications, and sometimes intravenous medications. Once the pressure is controlled, a laser procedure (laser iridotomy) is usually performed to create a new drainage hole in the iris.
- Reason: A sudden, rapid, and severe increase in the pressure inside the eye (intraocular pressure) due to a sudden blockage of the eye’s drainage angle. This is a medical emergency.
- Uveitis:
- Reason: Inflammation of the uvea, the middle layer of the eye that includes the iris (colored part), ciliary body (produces fluid), and choroid (layer of blood vessels). It can be caused by autoimmune diseases, infections, or trauma.
- Symptoms: Deep eye pain, redness (often concentrated around the iris), light sensitivity, blurred vision, and floaters.
- Treatment: The Eye Pain Reason for uveitis primarily involves:
- Steroid eye drops: To reduce inflammation.
- Dilating eye drops: To relieve pain and prevent iris adhesions.
- Oral steroids or other immunosuppressants may be needed for severe or recurrent cases, often managed by a rheumatologist in conjunction with an ophthalmologist.
- Reason: Inflammation of the uvea, the middle layer of the eye that includes the iris (colored part), ciliary body (produces fluid), and choroid (layer of blood vessels). It can be caused by autoimmune diseases, infections, or trauma.
- Optic Neuritis:
- Reason: Inflammation of the optic nerve, the bundle of nerve fibers that transmit visual information from the eye to the brain. It’s often associated with Multiple Sclerosis (MS) or viral infections.
- Symptoms: Pain behind the eye, often worsened by eye movement, accompanied by rapid vision loss (which can range from mild blurring to severe loss), and dulled color vision.
- Treatment: Often involves high-dose intravenous steroids, which can speed visual recovery but may not alter the overall long-term outcome. Treatment also focuses on managing the underlying cause, if identified.
- Reason: Inflammation of the optic nerve, the bundle of nerve fibers that transmit visual information from the eye to the brain. It’s often associated with Multiple Sclerosis (MS) or viral infections.
- Sinusitis / Migraine (Referred Pain):
- Reason: Pain originating from inflamed sinuses or a severe headache condition like migraine can be felt in or around the eyes. This is referred to as pain, meaning the eye itself is not the primary problem.
- Symptoms: Pain around or behind the eye, often accompanied by pressure, facial pain, nasal congestion (sinusitis), or throbbing headache, light sensitivity, and nausea (migraine). The eye may not show significant redness or discharge.
- Treatment: The Eye Pain Reason for this type of pain involves addressing the underlying condition:
- Sinusitis: Antibiotics, decongestants, nasal sprays, and warm compresses.
- Migraine: Pain relievers, triptans, or other migraine-specific medications.
- Sinusitis: Antibiotics, decongestants, nasal sprays, and warm compresses.
- Reason: Pain originating from inflamed sinuses or a severe headache condition like migraine can be felt in or around the eyes. This is referred to as pain, meaning the eye itself is not the primary problem.
- Scleritis / Episcleritis:
- Reason: Inflammation of the sclera (the white outer wall of the eye, scleritis) or the episclera (a thin layer of tissue on top of the sclera, episcleritis). Scleritis is much more severe and often associated with systemic autoimmune diseases (e.g., rheumatoid arthritis, lupus).
- Symptoms:
- Episcleritis: Mild to moderate localized pain, redness (often a sector of the white of the eye), tenderness. Usually benign and self-limiting.
- Scleritis: Deep, constant, severe, boring eye pain that can radiate to the temple or jaw. The eye is usually intensely red, and redness may not blanch with eye drops. It can also cause light sensitivity and blurred vision.
- Episcleritis: Mild to moderate localized pain, redness (often a sector of the white of the eye), tenderness. Usually benign and self-limiting.
- Treatment:
- Episcleritis: Often resolves on its own or with topical anti-inflammatory drops.
- Scleritis: Requires aggressive treatment with oral anti-inflammatory drugs (NSAIDs), oral steroids, or immunosuppressants, often in collaboration with a rheumatologist, to prevent vision loss and manage underlying systemic disease.
- Episcleritis: Often resolves on its own or with topical anti-inflammatory drops.
- Reason: Inflammation of the sclera (the white outer wall of the eye, scleritis) or the episclera (a thin layer of tissue on top of the sclera, episcleritis). Scleritis is much more severe and often associated with systemic autoimmune diseases (e.g., rheumatoid arthritis, lupus).
Suffering from persistent eye pain? Book an appointment with our eye specialist today for accurate diagnosis and effective treatment.
Book Appointment TodayWhen to Seek Medical Attention for Eye Pain
Any severe, persistent, or worsening eye pain warrants a professional evaluation by an ophthalmologist. Never self-diagnose severe eye pain.
Seek immediate emergency medical attention if your eye pain is accompanied by:
- Sudden, significant vision loss.
- Severe eye pain that is excruciating or debilitating.
- Seeing halos around lights.
- Nausea and vomiting with eye pain.
- A foreign object embedded in your eye.
- Recent eye trauma or injury.
- One eye bulged out.
- Sudden double vision.
Schedule a prompt consultation with an ophthalmologist (urgent, but not necessarily emergency room) if:
- Your eye pain persists for more than a day or two without improvement.
- You notice any changes in your vision (blurry, cloudy).
- There is pus-like or excessive discharge from your eye.
- Your eye pain is accompanied by extreme light sensitivity.
- If you wear contact lenses and develop any eye pain or redness.
- You suspect any form of infection.
- You simply aren’t sure about the cause of your eye pain.
Home Care for Mild Eye Pain
For very mild eye irritation or discomfort that you suspect is due to eye strain, mild dry eyes, or a minor foreign body that has already flushed out, you can try these home care tips before seeking medical attention:
- Rest your eyes: Close them for a few minutes, or reduce screen time.
- Warm or cool compresses: Apply a clean, damp cloth to your closed eyelids. Warm for styes/blepharitis, cool for general irritation/allergy.
- Artificial tears: Over-the-counter lubricating eye drops can provide temporary relief for dryness or irritation.
- Avoid rubbing: This can worsen irritation and cause damage.
- Ensure good lighting: When reading or using screens, make sure you have adequate, glare-free lighting.
Your Vision, Our Priority: Expert Care at Indira Gandhi Eye Hospitals
Eye pain is a signal from your body, and understanding its Eye Pain Reason is essential for effective care and preserving your vision. While some causes are minor, others can threaten your eyesight if not addressed promptly. Never underestimate persistent or severe eye pain.
At Indira Gandhi Eye Hospitals, our dedicated team of experienced ophthalmologists is equipped with state-of-the-art diagnostic tools and expertise to accurately pinpoint the cause of your eye pain. We offer a comprehensive range of treatments, from managing common irritations to advanced surgical interventions for complex conditions, all tailored to your specific needs. Your eye health is our utmost priority, and we are committed to providing you with compassionate, expert care.
If you are experiencing eye pain and are concerned about its Eye Pain Reason, please do not hesitate to reach out. For consultations, precise diagnosis, and comprehensive treatment options, visit our website at https://indiragandhiehospital.com/ to learn more or schedule an appointment. Let Indira Gandhi Eye Hospitals be your trusted partner in maintaining healthy, comfortable, and clear vision.
Suffering from persistent eye pain? Book an appointment with our eye specialist today for accurate diagnosis and effective treatment.
Book Appointment TodayFrequently Asked Questions (FAQs)
What are the most common reasons for experiencing eye pain?
The most common reasons for eye pain are often related to the eye’s surface, including foreign bodies (like dust or eyelashes), conjunctivitis (pink eye), dry eye syndrome, and corneal abrasions or ulcers. These vary from mild irritation to severe discomfort, with varied Eye Pain Reason
When should I be worried about eye pain and seek immediate medical help?
You should seek immediate medical help if eye pain is sudden, severe, accompanied by significant vision loss, seeing halos around lights, nausea, vomiting, or if you suspect an object is embedded in your eye or there has been recent trauma. These could indicate serious and time-sensitive conditions requiring urgent Eye Pain Reason
Can eye pain be a symptom of a problem not directly in the eye, like a headache or sinus issue?
Yes, eye pain can indeed be referred pain from other areas. Conditions like sinusitis (inflamed sinuses) or migraines (severe headaches) can cause pain that feels like it’s in or behind the eye, often without any visible eye abnormalities, requiring their specific Eye Pain Reason
Is it safe to use over-the-counter eye drops for any type of eye pain?
Over-the-counter artificial tears can provide temporary relief for mild irritation or dry eyes, but they are not suitable for all types of eye pain. For severe pain, pain with vision changes, or pain with thick discharge, using over-the-counter drops without professional diagnosis can delay crucial treatment and potentially worsen the condition.
What’s the biggest difference in treatment for viral versus bacterial pink eye?
The key difference in Eye Pain Reason | Treatment for pink eye lies in their cause; viral pink eye typically only requires supportive care like cold compresses and artificial tears as it resolves on its own, whereas bacterial pink eye necessitates antibiotic eye drops or ointment prescribed by a doctor.
Can wearing contact lenses cause severe eye pain, and what should I do if it happens?
Yes, improper contact lens use, overwearing, or poor hygiene can lead to severe eye pain due to corneal abrasions or infections (ulcers). If you experience severe eye pain while wearing contact lenses, remove them immediately and seek urgent medical attention, as it could be a serious infection requiring prompt Eye Pain Reason