|
Getting your Trinity Audio player ready...
|
Living with diabetes can feel like juggling many different health aspects at once. You’re constantly mindful of your blood sugar, diet, activity levels, and perhaps even your foot care. But there’s another crucial area that deserves your unwavering attention and proactive care: your eyes. Diabetes, if not well-managed, can quietly, yet profoundly, impact your vision, potentially leading to serious and irreversible damage.
It’s a stark reality, but the good news is that understanding How Diabetes Affects Eyes and diligently implementing prevention tips can make a world of difference. Vision loss from diabetes is often preventable, and armed with the right knowledge and commitment, you can significantly reduce your risk. Today, we’re going to delve deep into the intricate ways diabetes impacts your precious eyesight, explore the symptoms to watch out for, and most importantly, equip you with actionable prevention strategies. At Indira Gandhi Eye Hospitals, we believe that informed patients are empowered patients, especially when it comes to safeguarding your vision against the challenges of diabetes.
The Root Cause: Uncontrolled Blood Sugar’s Impact on Eyes
To truly grasp How Diabetes Affects Eyes, we must first understand the fundamental problem: persistently high levels of glucose (sugar) in your blood, a condition known as hyperglycemia. Diabetes, whether Type 1 or Type 2, means your body isn’t effectively producing or utilizing insulin to keep blood sugar levels balanced. Over time, this chronic exposure to high sugar levels takes a toll on the intricate network of blood vessels throughout your body.
The most vulnerable of these are the tiny, delicate blood vessels, known as capillaries. Your eyes, particularly the retina – the light-sensitive tissue at the back of your eye responsible for converting light into electrical signals for your brain – are incredibly rich in these microscopic vessels. When these small vessels are subjected to prolonged high sugar, they become damaged. They can swell, weaken, leak fluid, or even become completely blocked. This damage initiates a cascade of problems that ultimately jeopardize your vision. This microvascular damage is the insidious starting point for many diabetic eye complications.
Worried about how diabetes affects your eyes?
Early detection is key! Schedule an eye check-up today to prevent complications and protect your vision.
Book Eye Check-UpUnderstanding Specific Eye Conditions: How Diabetes Affects Eyes in Detail
Diabetes doesn’t just impact your eyes in one way; it can lead to several distinct conditions, each with its own set of challenges. Knowing these conditions and their symptoms is key to understanding How Diabetes Affects Eyes and what to watch out for.
1. Diabetic Retinopathy (DR): The Leading Cause of Vision Loss
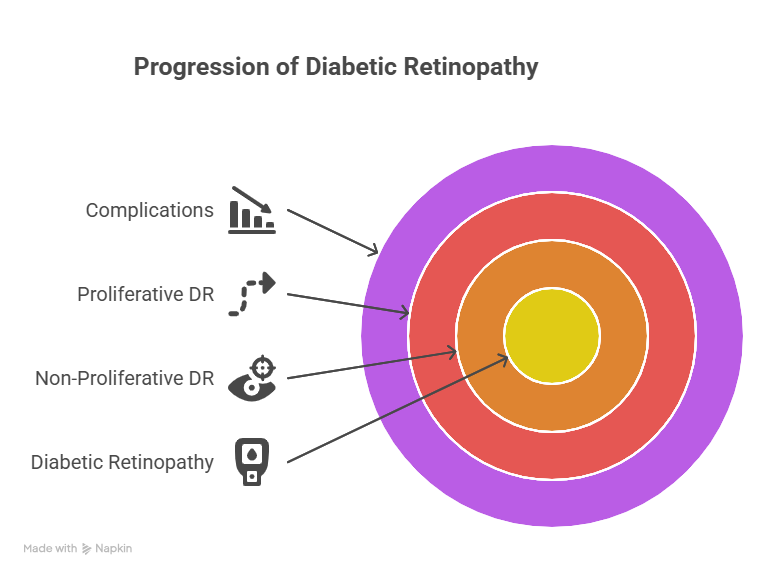
Diabetic retinopathy is the most common and serious eye complication of diabetes, and it’s the leading cause of blindness in working-age adults worldwide. It’s a progressive disease that develops when the blood vessels in the retina are damaged by high blood sugar.
- Non-Proliferative Diabetic Retinopathy (NPDR) – Early Stages:
- This is the initial stage, and it’s often called “background retinopathy.” The damage is confined to the retina, and vision is usually unaffected, making it asymptomatic in its early phases.
- Microaneurysms: These are tiny bulges or balloon-like swellings that form on the walls of the smallest retinal blood vessels. They are the earliest signs of DR and can sometimes leak small amounts of fluid or blood.
- Hemorrhages: Small spots of bleeding (dot and blot hemorrhages) can appear in the retina due to ruptured weak vessels.
- Hard Exudates: As blood vessels leak, fats and proteins can deposit in the retina, forming yellow or white deposits called hard exudates.
- Cotton Wool Spots: These are fluffy, white spots on the retina that indicate areas where nerve fibers have been damaged due to inadequate blood supply.
- NPDR can be classified as mild, moderate, or severe depending on the extent of these changes. In the severe NPDR stage, many blood vessels become blocked, signaling a high risk of progression to the more advanced form.
- This is the initial stage, and it’s often called “background retinopathy.” The damage is confined to the retina, and vision is usually unaffected, making it asymptomatic in its early phases.
- Proliferative Diabetic Retinopathy (PDR) – Advanced Stage:
- This is the more advanced and vision-threatening stage of DR. It occurs when large areas of the retina are deprived of oxygen due to widespread blood vessel damage and blockage.
- Neovascularization: In response to the lack of oxygen, the retina desperately tries to grow new blood vessels. However, these new vessels (neovascularization) are abnormal, fragile, and weak. They often grow on the surface of the retina or into the vitreous gel (the clear, jelly-like substance that fills the eye).
- Vitreous Hemorrhage: These fragile new blood vessels are prone to bleeding. If they rupture, blood can leak into the vitreous gel, causing floaters (dark spots or strings that drift across your vision) or sudden, severe vision loss.
- Tractional Retinal Detachment: The abnormal new vessels are often accompanied by scar tissue. This scar tissue can contract and pull on the retina, causing it to detach from the back of the eye. Retinal detachment is a serious condition that can lead to permanent blindness if not treated promptly.
- Neovascular Glaucoma: In severe PDR, abnormal new blood vessels can grow on the iris (the colored part of the eye) and into the drainage angle of the eye. This blocks the natural fluid drainage system, leading to a sudden and dangerous rise in eye pressure, causing a very painful and aggressive form of glaucoma.
- Symptoms of DR: In early NPDR, there are typically no symptoms. As it progresses, especially into PDR or if DME develops, your symptoms may include blurred vision, floaters, dark spots in vision, sudden vision loss, or difficulty seeing at night.
- This is the more advanced and vision-threatening stage of DR. It occurs when large areas of the retina are deprived of oxygen due to widespread blood vessel damage and blockage.
Worried about how diabetes affects your eyes?
Early detection is key! Schedule an eye check-up today to prevent complications and protect your vision.
Book Eye Check-Up2. Diabetic Macular Edema (DME): Affecting Your Central Vision
Diabetic macular edema (DME) is a common cause of vision loss in people with diabetic retinopathy. It can occur at any stage of DR, even in early NPDR.
- Mechanism: DME develops when fluid and fat leak from damaged blood vessels in the retina and accumulate in the macula. The macula is the small, central part of the retina responsible for sharp, detailed central vision – what you use for reading, recognizing faces, and driving.
- Symptoms: DME leads to blurred central vision, distorted images (e.g., straight lines appearing wavy or bent), and difficulty with tasks requiring fine detail. It can significantly impact your ability to perform daily activities.
3. Cataracts: Accelerated Clouding of the Lens
While cataracts are a natural part of aging for everyone, diabetes can cause them to develop at a younger age and progress more rapidly.
- Mechanism: High blood sugar levels can lead to the accumulation of sorbitol (a sugar alcohol) in the lens, causing swelling and damage to its proteins. This leads to the lens becoming cloudy and opaque.
- Symptoms: Cataracts cause blurred or cloudy vision, increased sensitivity to glare (especially from headlights at night), fading or yellowing of colors, and frequent changes in eyeglass prescriptions.
4. Glaucoma: Increased Risk and Specific Forms
People with diabetes have a higher risk of developing glaucoma, a group of diseases that damage the optic nerve, often due to high pressure inside the eye.
- Open-Angle Glaucoma: The most common form, where the eye’s drainage angle is open but fluid doesn’t drain efficiently, leading to a gradual buildup of pressure. Diabetes increases the risk for this common type. It typically has no early symptoms.
- Neovascular Glaucoma: This is a more severe and specific type of glaucoma strongly linked to advanced PDR. As mentioned above, the abnormal new blood vessels can grow on the iris and into the drainage angle, blocking fluid outflow and causing a rapid, painful rise in eye pressure.
- Symptoms: For open-angle glaucoma, vision loss is gradual and affects peripheral vision first, often without noticeable symptoms until advanced. For neovascular glaucoma, symptoms include severe eye pain, redness, sudden vision loss, and seeing halos around lights, often accompanied by headache, nausea, and vomiting.
5. Other Issues: Fluctuating Vision and Infections
- Fluctuating Vision: Rapid changes in blood sugar levels can temporarily affect the shape of the eye’s lens, leading to blurry vision that comes and goes. This is usually temporary and resolves once blood sugar stabilizes.
- Increased Susceptibility to Infections: Diabetes can weaken the immune system, making individuals more prone to eye infections like styes (a painful lump on the eyelid) or conjunctivitis (pink eye).
Understanding How Diabetes Affects Eyes through these specific conditions highlights the urgency of preventive measures.
Proactive Prevention: Crucial Tips to Protect Your Vision
The good news is that vision loss from diabetes is largely preventable. The key is a multi-faceted approach focusing on rigorous diabetes management and consistent eye care. These prevention tips are your most powerful tools against How Diabetes Affects Eyes.
Worried about how diabetes affects your eyes?
Early detection is key! Schedule an eye check-up today to prevent complications and protect your vision.
Book Eye Check-UpA. Optimal Blood Sugar Control: The Absolute Cornerstone
This is the most critical step. Maintaining your blood glucose levels as close to your target range as possible is paramount.
- HbA1c Target: Work with your doctor to achieve and maintain an HbA1c level (a measure of your average blood sugar over the past 2-3 months) generally below 7%, or as specifically recommended for your health. Each percentage point reduction in HbA1c significantly lowers the risk of diabetic eye disease progression.
- Daily Monitoring: Regularly check your fasting, pre-meal, and post-meal blood glucose levels to understand daily fluctuations and make timely adjustments to your diet, medication, and activity.
- Strategies: Adhere strictly to your prescribed diabetes medications (oral medications, insulin), follow a consistent, balanced dietary plan (focus on whole foods, limit refined sugars and processed carbohydrates), and engage in regular physical activity. Avoid large blood sugar spikes and crashes.
B. Rigorous Blood Pressure Management: A Vital Partner
High blood pressure (hypertension) acts as an accomplice to high blood sugar, significantly accelerating damage to the delicate blood vessels in your eyes.
- Why it Matters: Uncontrolled high blood pressure adds extra stress to the already fragile capillaries in your retina, making them more prone to leakage, rupture, and blockages, thereby worsening diabetic retinopathy.
- Target Blood Pressure: Aim for a blood pressure reading generally below 130/80 mmHg, or as specifically advised by your doctor based on your overall health.
- Strategies: This often involves a combination of prescribed blood pressure medications, a low-sodium diet (like the DASH diet), regular exercise, and stress management techniques. Regular home blood pressure monitoring is also highly recommended.
C. Cholesterol and Lipid Control: Supporting Vascular Health
High levels of cholesterol and other fats (lipids) in the blood can contribute to overall vascular disease, which impacts your eye health.
- Why it Matters: High cholesterol can lead to plaque buildup in blood vessels (atherosclerosis), further impairing blood flow to the eyes. Additionally, leaked lipids can deposit in the retina, worsening macular edema and other retinal damage.
- Target Levels: Work with your doctor to achieve healthy levels of LDL (“bad” cholesterol), HDL (“good” cholesterol), and triglycerides.
- Strategies: This includes a heart-healthy diet rich in fruits, vegetables, whole grains, and healthy fats while limiting saturated and trans fats. Regular exercise and, if necessary, cholesterol-lowering medications (like statins) play an important role.
D. Regular Comprehensive Dilated Eye Exams: Your Essential Shield
This is the single most powerful diagnostic tool against the impact of How Diabetes Affects Eyes.
- Frequency:
- Type 1 Diabetes: First dilated eye exam within 5 years of diagnosis.
- Type 2 Diabetes: First dilated eye exam shortly after diagnosis (as Type 2 often goes undiagnosed for years, and damage may already be present).
- Both Types: After the initial exam, most individuals with diabetes should have a comprehensive dilated eye exam at least once a year, or more frequently if signs of retinopathy are detected or if blood sugar control is poor.
- Type 1 Diabetes: First dilated eye exam within 5 years of diagnosis.
- What Happens: During a dilated eye exam, your ophthalmologist uses special eye drops to widen your pupils. This allows a much clearer and magnified view of your retina, optic nerve, and the delicate blood vessels. They will meticulously check for the earliest signs of damage, such as microaneurysms, hemorrhages, fluid leakage, swelling (macular edema), or abnormal new blood vessel growth.
- Advanced Imaging (If Needed): Your doctor may also use Optical Coherence Tomography (OCT) to get highly detailed cross-sectional images of your retina and measure any swelling. Fluorescein Angiography, which involves injecting a dye into your arm to highlight retinal blood vessels, can also be used to detect leakage or abnormal growth patterns. versible damage.
Worried about how diabetes affects your eyes?
Early detection is key! Schedule an eye check-up today to prevent complications and protect your vision.
Book Eye Check-UpE. Embrace a Healthy Lifestyle: Holistic Protection
These broader lifestyle factors significantly complement your medical management and contribute to your overall health, directly benefiting your eyes.
- Quit Smoking: Smoking is a major accelerator of all diabetic complications. It significantly damages blood vessels throughout the body, including the eyes, and dramatically increases your risk of severe vision loss from diabetic retinopathy and other eye conditions. Quitting smoking is one of the most impactful things you can do for your eye health.
- Balanced, Diabetes-Friendly Diet: Focus on a diet rich in whole, unprocessed foods. Include plenty of fruits, vegetables (especially leafy greens for antioxidants), lean proteins, and healthy fats. Limit processed foods, sugary drinks, refined grains, and unhealthy saturated/trans fats. A registered dietitian can provide personalized guidance.
- Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, combined with muscle-strengthening activities. Exercise improves insulin sensitivity, helps control blood sugar, blood pressure, and weight – all crucial factors in preventing diabetic eye damage.
- Maintain a Healthy Weight: Losing even a modest amount of weight if you are overweight or obese can significantly improve insulin sensitivity and help you manage your blood sugar, blood pressure, and cholesterol, thereby contributing to better eye health outcomes.
When to Seek Medical Care & Treatment Options
The best treatment is always prevention. However, if diabetic eye disease does develop, modern ophthalmology offers effective treatments to manage the conditions and preserve vision, particularly when detected early. These include:
- Laser Photocoagulation: Used to seal leaky blood vessels (focal laser for DME) or to destroy abnormal new blood vessels and prevent their growth (panretinal photocoagulation for PDR).
- Intravitreal Injections: Medications (e.g., Anti-VEGF agents or steroids) are injected into the eye to reduce swelling in the macula (DME) or to inhibit the growth of abnormal blood vessels (PDR).
- Vitrectomy Surgery: For advanced complications like severe vitreous hemorrhage or tractional retinal detachment, a surgical procedure called vitrectomy may be performed to remove blood and scar tissue from the eye.
- Cataract Surgery: For diabetic cataracts that significantly impair vision, surgical removal of the cloudy lens and replacement with an artificial one can restore clear vision.
These treatments are powerful, but they work best when the disease is caught in its earlier, more manageable stages.
The Power of a Collaborative Team
Managing diabetes and preventing its eye complications is a collaborative effort. You are at the center of your care team, but you’ll benefit immensely from working closely with:
- Your Endocrinologist or General Practitioner is for overall diabetes management.
- Your Ophthalmologist for specialized eye care, regular exams, and specific treatments.
- A Registered Dietitian for personalized nutritional guidance.
This multidisciplinary approach ensures all aspects of your health are monitored, providing the best defense against How Diabetes Affects Eyes.
Your Vision, Our Priority: Expert Care at Indira Gandhi Eye Hospitals
Understanding How Diabetes Affects Eyes is the first step towards preserving your vision. While the threat is real, the message is one of hope and empowerment. By taking proactive steps to rigorously manage your blood sugar, blood pressure, and cholesterol, embracing a healthy lifestyle, and committing to regular, comprehensive dilated eye examinations, you are equipping yourself with the best possible defense against vision loss.
At Indira Gandhi Eye Hospitals, our dedicated team of experienced ophthalmologists specializes in diagnosing, treating, and, crucially, helping you prevent diabetic eye diseases. We are equipped with state-of-the-art diagnostic tools and offer a full spectrum of advanced treatments, from cutting-edge laser therapies and injections to complex surgical procedures, all tailored to your individual needs. We are here to partner with you every step of the way, ensuring your eyes receive the expert care they deserve.
For a comprehensive eye examination, personalized advice, or any concerns regarding How Diabetes Affects Eyes and your ocular health, please do not hesitate to reach out. Visit our website at https://indiragandhieyehospital.com/ to learn more or to schedule an appointment. Let Indira Gandhi Eye Hospitals be your trusted partner in maintaining a healthy and clear vision for life.
Worried about how diabetes affects your eyes?
Early detection is key! Schedule an eye check-up today to prevent complications and protect your vision.
Book Eye Check-UpFrequently Asked Questions (FAQs)
How does high blood sugar specifically damage the eyes in diabetic retinopathy?
High blood sugar damages the tiny blood vessels in the retina, causing them to swell, leak fluid, or become blocked. This impairs blood flow and oxygen supply to the retina, leading to the growth of abnormal, fragile new blood vessels that can bleed or cause scarring, impacting vision.
Will I notice symptoms right away if diabetes starts affecting my eyes?
No, sadly, early diabetic eye disease, especially non-proliferative diabetic retinopathy, often has no noticeable symptoms. Vision changes typically occur only in the more advanced stages or when diabetic macular edema develops, which is why regular dilated eye exams are crucial for early detection.
How often should someone with diabetes get a comprehensive eye exam?
Individuals with Type 2 diabetes should have their first comprehensive dilated eye exam soon after diagnosis, and those with Type 1 within five years of diagnosis. Subsequently, both should have an exam at least once a year, or more frequently if advised by their ophthalmologist.
Can improving my blood sugar control reverse existing eye damage from diabetes?
While excellent blood sugar control can significantly slow the progression of diabetic eye disease and sometimes even lead to minor improvements in early stages, it generally cannot reverse significant damage or restore vision that has already been lost due to advanced complications. Early detection is key to preventing this irreversible damage.
What are the main treatments if diabetic retinopathy is detected?
If diabetic retinopathy is detected, treatments may include laser photocoagulation to seal leaky vessels or destroy abnormal ones, and intravitreal injections of medications (such as Anti-VEGF agents or steroids) to reduce swelling or inhibit new blood vessel growth. In advanced cases, vitrectomy surgery may be needed.
Does diabetes increase the risk of eye conditions other than retinopathy?
Yes, diabetes also increases the risk of developing cataracts at a younger age, and can lead to a specific and severe form of glaucoma called neovascular glaucoma. It can also cause temporary blurry vision due to fluctuating blood sugar levels affecting the eye’s lens.