|
Getting your Trinity Audio player ready...
|
Diabetes, as you might know, is a condition that impacts nearly every part of your body. When we hear “diabetes,” our minds often go straight to blood sugar levels, diet, or perhaps even foot care. But there’s another crucial area that deserves your unwavering attention: your eyes. Your vision is a precious gift, and for individuals living with diabetes, safeguarding it becomes an even more critical mission.
The good news is, while diabetes does pose a significant risk to your eyesight, there are powerful and proactive steps you can take. Today, we’re going to dive deep into understanding How To Prevent Eye Damage From Diabetes, exploring the specific ways this condition can affect your vision, and most importantly, the comprehensive strategies you can implement to protect your eyes for years to come. At Indira Gandhi Eye Hospitals, we believe that education and early action are your strongest allies in this journey.
The Unseen Threat: How Diabetes Harms Your Eyes
Diabetes affects the body’s ability to produce or use insulin effectively, leading to persistently high levels of glucose (sugar) in the blood. While seemingly benign, this sustained high blood sugar acts as a silent, insidious threat to the delicate network of blood vessels throughout your body, particularly the tiny ones (capillaries). Your eyes, being incredibly rich in these microscopic blood vessels, are particularly vulnerable.
The damage to these tiny blood vessels is known as microvascular complications. In the eye, this primarily impacts the retina, the light-sensitive tissue at the back of your eye, responsible for sending visual information to your brain. This specific type of damage is called diabetic retinopathy, and it’s the leading cause of blindness in working-age adults. But diabetic damage isn’t limited to the retina; it can also accelerate the development of cataracts and glaucoma, further jeopardizing your vision.
The danger lies in the fact that How To Prevent Eye Damage From Diabetes often starts without any noticeable symptoms. You might have significant damage occurring in your eyes long before you experience any changes in your vision. This silent progression underscores the absolute necessity of proactive management and regular eye care.
Protect your sight — book a diabetic eye screening at Indira Gandhi Eye Hospital today; early detection can save your vision.
Book Appointment TodayUnderstanding Diabetic Eye Diseases: The Specifics
To truly grasp How To Prevent Eye Damage From Diabetes, let’s first understand the specific conditions diabetes can cause:
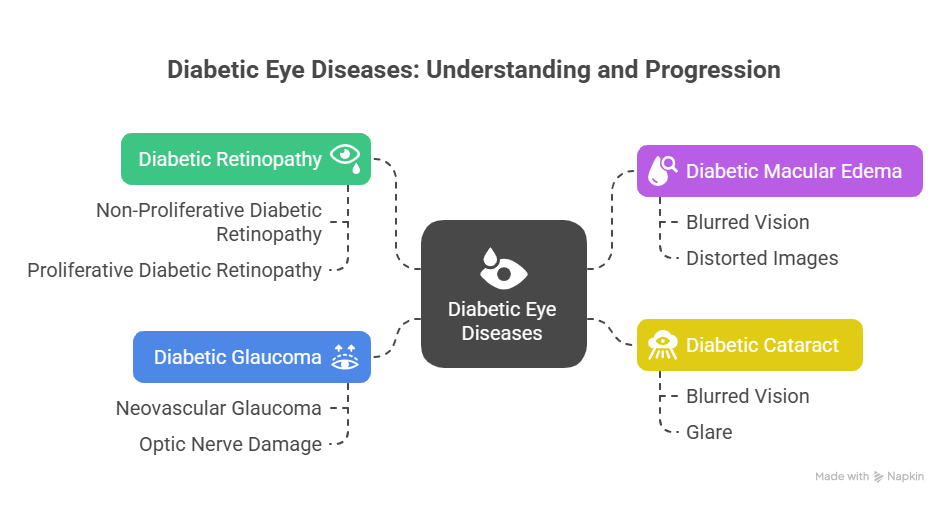
- Diabetic Retinopathy: This is the most common and serious diabetic eye disease, caused by damage to the blood vessels in the retina. It progresses through stages:
- Non-Proliferative Diabetic Retinopathy (NPDR) – Early Stage:
- Microaneurysms: Tiny bulges in the blood vessels, like small balloons, which can leak fluid or blood.
- Hemorrhages: Small bleeding spots in the retina.
- Hard Exudates: Fatty deposits that leak from damaged vessels.
- Cotton Wool Spots: Areas of nerve fiber damage in the retina caused by poor blood flow.
- At this stage, vision is often unaffected, making regular screening vital for early detection.
- Proliferative Diabetic Retinopathy (PDR) – Advanced Stage:
- Neovascularization: This is the hallmark of PDR. The severely damaged retina tries to compensate for lack of oxygen by growing new, abnormal, fragile blood vessels (neovascularization) on the surface of the retina or optic nerve. These new vessels are weak and prone to bleeding.
- Vitreous Hemorrhage: If these new, fragile vessels bleed, blood can fill the vitreous gel (the clear, jelly-like substance that fills the eye), causing sudden, severe vision loss or floaters.
- Retinal Detachment: The abnormal vessels can also form scar tissue, which can contract and pull on the retina, leading to retinal detachment – a serious condition that can cause permanent blindness if not treated promptly.
- Neovascular Glaucoma: In severe cases, these abnormal blood vessels can grow on the iris (the colored part of the eye) and block the drainage angle of the eye, leading to a dangerous rise in eye pressure, known as neovascular glaucoma. This is a very painful and aggressive form of glaucoma.
- Non-Proliferative Diabetic Retinopathy (NPDR) – Early Stage:
- Diabetic Macular Edema (DME):
- This can occur at any stage of diabetic retinopathy. It happens when fluid and fats leak from damaged blood vessels into the macula, the central part of the retina responsible for sharp, detailed central vision (what you use to read, recognize faces, and see colors).
- Impact: Macular edema causes blurred central vision, distorted images, and difficulty reading or seeing fine details. It’s a common cause of vision loss in people with diabetes.
- Diabetic Cataract:
- What it is: A cataract is a clouding of the eye’s natural lens, which normally works to focus light. While cataracts are a natural part of aging, people with diabetes tend to develop them at a younger age and experience faster progression.
- Mechanism: High blood sugar levels can cause swelling in the lens and damage to its proteins, leading to clouding.
- Impact: Blurred vision, glare, difficulty with night vision, and colors appearing faded.
- Diabetic Glaucoma (Neovascular Glaucoma):
- What it is: Glaucoma is a group of eye conditions that damage the optic nerve, often due to abnormally high pressure inside the eye. Neovascular glaucoma, specifically linked to severe diabetic retinopathy, occurs when abnormal new blood vessels grow on the iris and in the drainage angle of the eye.
- Mechanism: These new vessels block the natural drainage system of the eye, leading to a dangerous spike in intraocular pressure, which damages the optic nerve.
- Impact: Can cause severe pain, redness, and rapid, irreversible vision loss if not managed aggressively.
Understanding these specific threats clarifies just how vital it is to learn How To Prevent Eye Damage From Diabetes proactively.
The Cornerstone of Prevention: How To Prevent Eye Damage From Diabetes
The overwhelming message from ophthalmologists and endocrinologists worldwide is clear: the best strategy for How To Prevent Eye Damage From Diabetes is through vigilant management of your diabetes itself, combined with consistent, specialized eye care. It’s a multi-pronged approach that puts you in the driver’s seat of your eye health.
A. Master Your Blood Sugar (Glycemic Control): This is the single most critical step. Consistently high blood sugar levels are the direct cause of microvascular damage.
- HbA1c Target: Work with your doctor to achieve and maintain an HbA1c level as close to normal as safely possible, often below 7% or even lower for some individuals. HbA1c provides an average blood sugar level over the past 2-3 months.
- Daily Glucose Monitoring: Regularly check your fasting and post-meal blood glucose levels to understand daily fluctuations and make immediate adjustments to diet or medication as needed.
- Mechanism: Tight glycemic control helps prevent and slow down the damage to the tiny blood vessels in your retina, significantly reducing the risk of developing or progressing diabetic retinopathy.
- Strategies: Adhere strictly to your prescribed diabetes medications, follow a balanced dietary plan (focus on low glycemic index foods, lean proteins, ample fiber, and limit processed sugars and refined carbohydrates), eat regular meals, and avoid drastic sugar spikes.
B. Control Your Blood Pressure (Hypertension Management): High blood pressure (hypertension) is a significant co-factor that dramatically accelerates diabetic eye damage.
- Why it matters: Just like high blood sugar, high blood pressure puts immense stress on the fragile blood vessels in your eyes, making them more prone to leakage and damage, thus worsening diabetic retinopathy.
- Target Blood Pressure: Aim for a blood pressure reading generally below 130/80 mmHg, or as specifically advised by your doctor based on your health profile.
- Strategies: This often involves a combination of prescribed medication, a low-sodium diet (e.g., DASH diet), regular physical activity, and stress management techniques. Regular monitoring at home is also beneficial.
C. Manage Your Cholesterol and Lipids: High levels of cholesterol and other fats in the blood can contribute to broader vascular damage and even directly impact the eyes.
- Why it matters: High cholesterol can lead to plaque formation (atherosclerosis) in blood vessels, further impairing blood flow to the eyes. Additionally, leaked fats (lipids) can deposit in the retina, worsening macular edema.
- Target Levels: Work with your doctor to achieve healthy levels of LDL (bad cholesterol), HDL (good cholesterol), and triglycerides.
- Strategies: This involves a heart-healthy diet rich in fruits, vegetables, whole grains, and healthy fats while limiting saturated and trans fats. Regular exercise and, if necessary, cholesterol-lowering medications (like statins) play a crucial role.
D. Regular Comprehensive Dilated Eye Exams: This is arguably the most powerful tool for How To Prevent Eye Damage From Diabetes that already exists, outside of managing the diabetes itself.
- Frequency: If you have Type 1 diabetes, you should typically have your first dilated eye exam within 5 years of diagnosis. For Type 2 diabetes, the first exam should be done shortly after diagnosis. After that, most individuals with diabetes should have a comprehensive dilated eye exam at least once a year, or more frequently if any signs of retinopathy are detected or if your blood sugar control is poor.
- What happens: During a dilated eye exam, your ophthalmologist will use special eye drops to widen your pupils, allowing a much clearer view of the retina and the blood vessels within it. They will use specialized equipment (like an ophthalmoscope, slit lamp) to look for the earliest signs of damage, such as microaneurysms, hemorrhages, fluid leakage, swelling (macular edema), or new blood vessel growth.
- Advanced Imaging (If Needed): Your doctor may also recommend Optical Coherence Tomography (OCT) to get highly detailed cross-sectional images of your retina and measure swelling, or Fluorescein Angiography, where a dye is injected into your arm to highlight blood vessels in your retina and detect leakage or abnormal growth.
- Asymptomatic Nature: Remember, early diabetic eye disease often has no symptoms. You won’t feel pain, and your vision might be clear. Regular exams are the only way to detect damage before it impacts your vision, allowing for timely intervention that can preserve your sight.
E. Embrace a Healthy Lifestyle: These lifestyle factors complement your medical management and contribute significantly to overall health, which directly impacts your eyes.
- Balanced, Diabetes-Friendly Diet: Focus on whole, unprocessed foods. Load up on a variety of fruits and vegetables (especially leafy greens rich in antioxidants), lean proteins, and healthy fats (from nuts, seeds, avocados, and olive oil). Limit processed foods, sugary drinks, refined grains, and unhealthy fats. A registered dietitian can provide personalized guidance.
- Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, along with muscle-strengthening activities. Exercise improves insulin sensitivity, helps control blood sugar, blood pressure, and weight, all of which are crucial for eye health.
- Quit Smoking: Smoking is a potent vasoconstrictor and greatly damages blood vessels throughout the body, including the eyes. It significantly worsens all diabetic complications and dramatically increases your risk of severe vision loss. Quitting smoking is one of the best things you can do for your eyes and overall health.
- Limit Alcohol Consumption: Excessive alcohol can affect blood sugar levels and contribute to other health issues that can indirectly impact eye health. Moderate consumption, if at all, is advisable.
- Maintain a Healthy Weight: Losing even a small amount of weight if you are overweight or obese can significantly improve insulin sensitivity and help manage blood sugar, blood pressure, and cholesterol, all contributing to better eye health.
Protect your sight — book a diabetic eye screening at Indira Gandhi Eye Hospital today; early detection can save your vision.
Book Appointment TodayWhen Damage Occurs: Treatment Options
Even with the best preventive efforts, sometimes eye damage from diabetes can occur or progress. The good news is that modern ophthalmology offers effective treatments to manage these conditions and prevent further vision loss. These treatments are often recommended by your eye specialist if they detect significant changes during your regular eye exams.
- Laser Photocoagulation:
- Focal Laser: Used for diabetic macular edema (DME) to seal specific leaking blood vessels, thereby reducing swelling in the macula.
- Panretinal Photocoagulation (PRP): Used for Proliferative Diabetic Retinopathy (PDR). This involves applying hundreds of tiny laser spots to the peripheral retina to destroy abnormal, fragile new blood vessels (neovascularization) and reduce their growth. This sacrifices some peripheral vision to save central vision.
- Focal Laser: Used for diabetic macular edema (DME) to seal specific leaking blood vessels, thereby reducing swelling in the macula.
- Intravitreal Injections:
- Anti-VEGF Injections: Medications (like Ranibizumab, Aflibercept, Bevacizumab) are injected directly into the vitreous jelly of the eye. They work by blocking a protein called Vascular Endothelial Growth Factor (VEGF), which is responsible for the growth of abnormal new blood vessels and leakage. These are highly effective for treating DME and PDR.
- Steroid Injections: Long-acting steroid medications can also be injected into the eye to reduce inflammation and swelling associated with DME.
- Anti-VEGF Injections: Medications (like Ranibizumab, Aflibercept, Bevacizumab) are injected directly into the vitreous jelly of the eye. They work by blocking a protein called Vascular Endothelial Growth Factor (VEGF), which is responsible for the growth of abnormal new blood vessels and leakage. These are highly effective for treating DME and PDR.
- Vitrectomy Surgery:
- This is a sophisticated surgical procedure performed for advanced complications of PDR, such as severe vitreous hemorrhage (blood filling the eye’s cavity) that doesn’t clear on its own, or tractional retinal detachment (where scar tissue pulls the retina away from the back of the eye). The surgeon removes the vitreous gel, clears the blood, removes scar tissue, and reattaches the retina.
- This is a sophisticated surgical procedure performed for advanced complications of PDR, such as severe vitreous hemorrhage (blood filling the eye’s cavity) that doesn’t clear on its own, or tractional retinal detachment (where scar tissue pulls the retina away from the back of the eye). The surgeon removes the vitreous gel, clears the blood, removes scar tissue, and reattaches the retina.
- Cataract Surgery:
- If a significant diabetic cataract forms and affects vision, surgical removal of the cloudy lens and replacement with a clear artificial intraocular lens (IOL) is performed. This can dramatically restore vision.
These treatments are powerful tools, but they work best when damage is detected early. This brings us full circle to the immense importance of knowing How To Prevent Eye Damage From Diabetes through proactive management and regular check-ups.
A Collaborative Approach: Your Healthcare Team
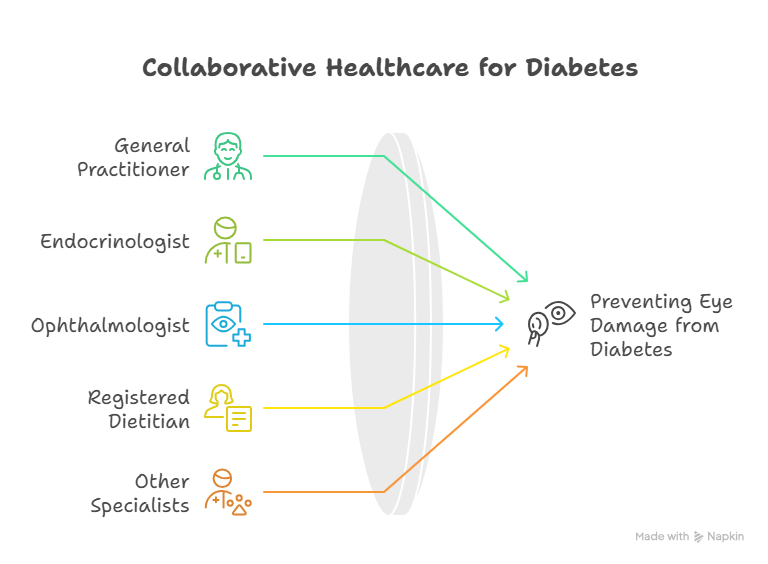
Effectively managing diabetes and preventing eye damage is a team effort. You are the most important player, but you’ll rely on a network of healthcare professionals:
- Your General Practitioner/Family Doctor: For overall health management and referrals.
- Your Endocrinologist: Specializes in diabetes management, medication, and blood sugar control.
- Your Ophthalmologist/Eye Specialist: Crucial for regular dilated eye exams, early detection of eye damage, and specialized treatment.
- A Registered Dietitian: To help you create a personalized meal plan for diabetes management.
- Other Specialists: As needed, such as a nephrologist (kidney specialist) or cardiologist (heart specialist), as diabetes often affects multiple organ systems.
Working closely with this team is paramount to understanding How To Prevent Eye Damage From Diabetes comprehensively.
Your Vision, Our Priority: Partnering for Eye Health at Indira Gandhi Eye Hospitals
Living with diabetes requires diligence, but it does not mean sacrificing your vision. By taking consistent, proactive steps to manage your blood sugar, blood pressure, and cholesterol, embracing a healthy lifestyle, and committing to regular, comprehensive dilated eye exams, you are doing everything in your power to protect your eyesight. Understanding How To Prevent Eye Damage From Diabetes is not just about avoiding complications; it’s about preserving your quality of life, your independence, and your ability to experience the world visually for years to come.
At Indira Gandhi Eye Hospitals, our dedicated team of ophthalmologists specializes in diagnosing, treating, and, crucially, helping you prevent diabetic eye diseases. We provide state-of-the-art diagnostic services and a full spectrum of treatment options, from advanced laser therapies and injections to complex surgical procedures, all tailored to your individual needs. We are here to partner with you every step of the way, ensuring your eyes receive the expert care they deserve.
For a comprehensive eye examination, personalized advice on How To Prevent Eye Damage From Diabetes, or to explore treatment options, we invite you to connect with us. Visit our website at https://indiragandhiehospital.com/ to learn more and schedule your appointment. Let Indira Gandhi Eye Hospitals be your steadfast ally in preserving your precious vision.
Protect your sight — book a diabetic eye screening at Indira Gandhi Eye Hospital today; early detection can save your vision.
Book Appointment TodayFrequently Asked Questions (FAQs)
What is the most important thing I can do to prevent eye damage from diabetes?
The single most crucial step is strict control of your blood sugar levels. Maintaining your HbA1c as close to your doctor’s target as safely possible is fundamental, as consistently high blood sugar directly damages the delicate blood vessels in your eyes.
How often should I get my eyes checked if I have diabetes?
If you have diabetes, you should undergo a comprehensive dilated eye examination at least once a year. Your ophthalmologist may recommend more frequent checks if you have existing signs of diabetic retinopathy or if your blood sugar control is not optimal.
Can eye damage from diabetes be reversed?
While some early changes, like mild swelling, can sometimes improve with excellent diabetes control, significant damage, especially scarring or permanent vision loss, often cannot be fully reversed. However, modern treatments can effectively prevent further progression and preserve remaining vision.
Do I need an eye exam even if my vision feels fine?
Absolutely, yes! Diabetic eye damage, particularly in its early and even moderate stages, often has no noticeable symptoms or impact on vision. A dilated eye exam is the only way for your ophthalmologist to detect these changes before they become severe and cause irreversible vision loss.
Besides blood sugar, what other factors are critical for preventing eye damage?
In addition to blood sugar control, managing your blood pressure and cholesterol levels is equally vital. High blood pressure and elevated cholesterol significantly worsen diabetic eye complications by putting extra strain on delicate eye vessels and contributing to further damage.
Are there any specific foods that can help prevent diabetic eye damage?
While no single food acts as a miracle cure, a diet rich in fruits, vegetables (especially leafy greens), whole grains, and lean proteins, while limiting processed foods, sugary drinks, and unhealthy fats, supports overall diabetes management and provides antioxidants beneficial for eye health.