|
Getting your Trinity Audio player ready...
|
Imagine looking through a window that has become increasingly foggy, scratched, or distorted over time. This is often the daily reality for someone whose cornea, the clear, outermost “window” of the eye, has been damaged by disease or injury. When this vital part of your eye loses its clarity or healthy function, it can profoundly impact your vision, making even simple tasks incredibly challenging.
The good news is that for many individuals facing such a challenge, there’s a remarkable solution that can restore crisp, clear sight: Cornea Transplant Surgery. This procedure, often considered one of the miracles of modern ophthalmology, involves replacing a diseased or damaged cornea with healthy donor tissue. It’s a journey that offers immense hope and the promise of seeing the world once again. Today, we’re going to delve deep into What is Cornea Transplant Surgery and its procedures, exploring why it’s needed, the different types of techniques involved, and what the recovery process entails. At Indira Gandhi Eye Hospitals, we are dedicated to guiding our patients through every step of this transformative journey, ensuring the highest standards of care and the best possible visual outcomes.
Understanding the Cornea: Your Eye’s Clear Window
Before we explore What is Cornea Transplant Surgery, let’s first appreciate the star of the show: the cornea. This small, transparent, dome-shaped tissue at the very front of your eye is vital for clear vision. Think of it as the eye’s primary focusing lens, responsible for about two-thirds of your eye’s total focusing power. Light enters your eye first through the cornea, which then bends (refracts) that light onto the lens and ultimately to the retina at the back of your eye.
The cornea’s remarkable clarity is due to its unique, highly organized structure and the absence of blood vessels. It receives its nutrients from the tear film on its surface and the aqueous humor (fluid) inside the eye. It has several distinct layers, each playing a crucial role:
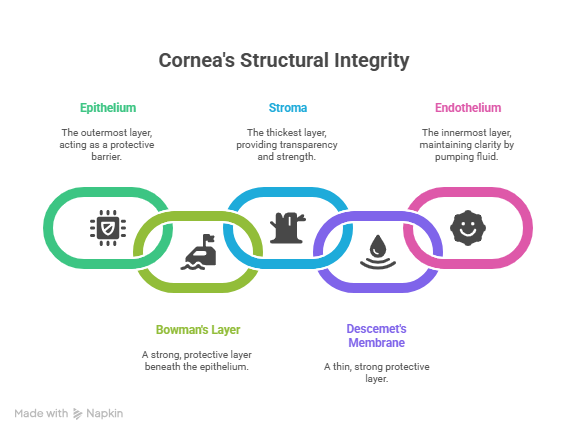
- Epithelium: The outermost layer, acting as a protective barrier against dust, bacteria, and water. It’s highly regenerative and heals quickly.
- Bowman’s Layer: A strong, protective layer beneath the epithelium.
- Stroma: The thickest layer, making up about 90% of the cornea’s thickness. It consists of highly organized collagen fibers, which are key to the cornea’s transparency and strength.
- Descemet’s Membrane: A thin, strong protective layer.
- Endothelium: The innermost layer, a single layer of specialized cells. These cells are crucial for maintaining the cornea’s clarity by actively pumping fluid out of the stroma, preventing swelling. Unlike epithelial cells, endothelial cells do not regenerate; once damaged, they are lost forever.
When any of these layers are compromised, the cornea can lose its transparency, become distorted, or swell, leading to blurred vision, glare, pain, and ultimately, significant vision impairment. This is when Cornea Transplant Surgery becomes a necessary and life-changing option.
Need clarity about Cornea Transplant Surgery?
Don’t let corneal problems affect your vision. Our eye specialists provide advanced cornea transplant care with safe and effective procedures. Book your consultation today to restore clear vision.
Book Cornea ConsultationWhy a Cornea Transplant Might Be Needed: When the Window Gets Cloudy
A cornea transplant, also known as keratoplasty, becomes necessary when the cornea is so damaged or diseased that it significantly impairs vision and cannot be effectively treated by other means (like eyeglasses, contact lenses, or simpler medical treatments). The reasons for needing Cornea Transplant Surgery are diverse and can affect different layers of the cornea:
- Keratoconus: This is one of the most common reasons for a cornea transplant. It’s a progressive eye disease in which the normally round, dome-shaped cornea thins and begins to bulge outward into a cone-like shape. This irregular shape causes significant distortion and blurring of vision that cannot be fully corrected with glasses or standard contact lenses. While milder cases can be managed with specialized contact lenses or corneal collagen cross-linking (which stiffens the cornea to prevent progression), advanced cases often require a transplant.
- Fuchs’ Dystrophy: This is a genetic condition that primarily affects the innermost layer of the cornea, the endothelium. The endothelial cells gradually die off, losing their ability to pump fluid out of the cornea. This leads to fluid buildup and swelling (edema) of the cornea, causing it to become cloudy and blurry, especially in the mornings. As the disease progresses, vision becomes persistently hazy.
- Corneal Scars: Scars on the cornea can result from various causes, including:
- Infections: Such as severe bacterial, fungal, or viral (herpes simplex or zoster) keratitis. These infections can leave opaque scar tissue.
- Injuries/Trauma: Accidents, chemical burns, or foreign bodies can cause permanent scarring.
- Previous Eye Surgery: Rarely, complications from other eye surgeries can lead to corneal scarring.
- Corneal Dystrophies: A group of rare, often genetic, conditions that cause abnormal material to build up in one or more layers of the cornea, leading to cloudiness or vision loss. Examples include lattice dystrophy, granular dystrophy, and macular dystrophy.
- Corneal Ulcers: Severe, non-healing infections that create an open sore on the cornea, leading to significant scarring and vision loss.
- Failed Previous Cornea Transplant: In some cases, a previously transplanted cornea might fail due to rejection, infection, or other complications, necessitating a second (or even third) transplant.
In all these scenarios, the common denominator is a loss of corneal transparency or structural integrity, leading to significantly impaired vision or severe pain that can only be resolved by replacing the damaged tissue. This clearly defines the necessity for Cornea Transplant Surgery.
What is Cornea Transplant Surgery? The Procedure Defined
Cornea Transplant Surgery (keratoplasty) is a surgical procedure that replaces part or all of a damaged cornea with healthy corneal tissue from a deceased human donor. It is one of the most common and successful transplant procedures performed today, with a high success rate in restoring vision.
The decision to undergo Cornea Transplant Surgery is made after a thorough evaluation by an ophthalmologist specializing in corneal diseases. This evaluation includes detailed eye examinations, imaging tests of the cornea, and a discussion of the patient’s overall health and vision goals.
Types of Cornea Transplant Surgery and Their Procedures: Precision in Layers
Modern Cornea Transplant Surgery and its procedures have evolved significantly. Instead of always replacing the entire cornea, surgeons can now often replace only the diseased layers, preserving healthy tissue. This leads to faster recovery, fewer complications, and better outcomes for many patients. The choice of procedure depends entirely on which layers of the cornea are affected.
Need clarity about Cornea Transplant Surgery?
Don’t let corneal problems affect your vision. Our eye specialists provide advanced cornea transplant care with safe and effective procedures. Book your consultation today to restore clear vision.
Book Cornea Consultation1. Penetrating Keratoplasty (PK) – Full-Thickness Cornea Transplant
- What it is: This is the traditional and oldest form of Cornea Transplant Surgery. In PK, the surgeon removes the entire central portion of the diseased cornea (all five layers) and replaces it with a full-thickness, clear donor cornea. The donor cornea is then meticulously sewn into place using very fine sutures (stitches), often numbering 16 or more.
- Indications: PK is typically performed for conditions affecting all layers of the cornea, such as advanced keratoconus with full-thickness scarring, severe corneal infections that have penetrated deeply, extensive corneal scarring from trauma, or when other partial-thickness transplants are not suitable.
- Procedure Overview:
- The patient receives local or general anesthesia.
- A trephine (a circular cutting instrument) is used to make a precise circular cut to remove the central, diseased portion of the patient’s cornea.
- A matching size donor cornea is prepared and carefully placed into the opening.
- The donor cornea is then secured with extremely fine nylon sutures, which are often left in place for many months or even years.
- Recovery: PK generally has the longest recovery time for vision, often taking 6-12 months or even longer for vision to stabilize, as the eye heals and astigmatism (irregular curvature) from the sutures resolves.
2. Lamellar Keratoplasty – Partial-Thickness Cornea Transplant
These procedures involve replacing only specific layers of the cornea, leaving healthy layers intact. This approach is revolutionizing Cornea Transplant Surgery and its procedures.
- A. Deep Anterior Lamellar Keratoplasty (DALK): For Stromal Diseases
- What it is: In DALK, the surgeon removes only the diseased front layers of the cornea (epithelium, Bowman’s layer, and most of the stroma), leaving the patient’s own healthy Descemet’s membrane and endothelium intact. A donor stroma is then placed and sutured into position.
- Indications: DALK is primarily performed for conditions that affect the front and middle layers of the cornea, such as keratoconus (where the endothelium is healthy), corneal dystrophies affecting the stroma, or superficial corneal scars.
- Procedure Overview:
- Anesthesia is administered.
- The surgeon carefully separates the diseased anterior layers of the cornea from the healthy Descemet’s membrane and endothelium. This often involves injecting a “big bubble” of air or fluid to achieve a clean separation.
- The diseased anterior layers are removed.
- A donor cornea that has had its Descemet’s membrane and endothelium removed is then carefully placed and sutured onto the patient’s remaining healthy posterior layers.
- Advantages: Because the patient’s own endothelium is preserved, the risk of endothelial rejection (the most common and serious type of rejection) is significantly reduced. This also leads to a stronger eye post-surgery and potentially faster visual recovery compared to PK, though sutures are still involved.
- B. Endothelial Keratoplasty (DSEK/DMEK): For Endothelial Diseases
- What it is: These are highly specialized procedures that replace only the innermost layer of the cornea (the endothelium) and Descemet’s membrane. The patient’s own healthy anterior and stromal layers are left untouched.
- Indications: Primarily performed for conditions affecting the endothelium, such as Fuchs’ Dystrophy or pseudophakic bullous keratopathy (corneal swelling after cataract surgery), where the rest of the cornea is clear.
- Procedure Overview (Simplified):
- Anesthesia is administered.
- The surgeon carefully strips away the diseased Descemet’s membrane and endothelium from the patient’s cornea through a tiny incision (usually 2-3mm).
- A very thin, delicate disc of donor Descemet’s membrane and endothelium (often pre-stripped by the eye bank for DMEK, or a slightly thicker graft for DSEK) is carefully prepared.
- This delicate donor graft is then folded or rolled and inserted into the eye through the small incision.
- Once inside the eye, an air bubble is injected to unfold the graft and press it against the back surface of the patient’s cornea, where it adheres naturally without sutures. The air bubble is typically left in the eye for several days, requiring the patient to lie flat on their back for much of the recovery period.
- Advantages: These procedures are truly revolutionary. Because only a very thin layer is replaced through a small incision and no sutures are used, vision recovery is often much faster (weeks to a few months) compared to PK or DALK. The risk of astigmatism is significantly lower, and the overall structural integrity of the eye is maintained. The risk of rejection is also lower than PK. DMEK is considered the most advanced form, offering the fastest and best visual outcomes due to its ultra-thin, single-cell layer graft, but it is technically more challenging.
Need clarity about Cornea Transplant Surgery?
Don’t let corneal problems affect your vision. Our eye specialists provide advanced cornea transplant care with safe and effective procedures. Book your consultation today to restore clear vision.
Book Cornea ConsultationThe Donor Cornea: A Gift of Sight
All corneal tissue used in Cornea Transplant Surgery comes from deceased human donors. These are individuals who, or whose families, have generously consented to organ and tissue donation. The donor corneas are meticulously screened and tested for diseases (like HIV, hepatitis) by eye banks, ensuring they are safe for transplantation. This rigorous screening process makes the risk of disease transmission extremely low. The availability of healthy donor corneas is entirely dependent on the generosity of donors and their families, making eye donation a profound gift of sight.
The Surgical Process: What to Expect
The journey through Cornea Transplant Surgery and its procedures typically involves several key stages:
- Pre-operative Evaluation: A thorough eye examination, including detailed imaging of the cornea, visual acuity tests, and a review of your medical history. Your ophthalmologist will discuss the best type of transplant for your condition, potential risks, benefits, and expected recovery.
- The Surgery:
- Performed in a sterile operating room, usually as an outpatient procedure (meaning you go home the same day).
- Anesthesia (local with sedation or general) will be administered to ensure you are comfortable and pain-free.
- The specific steps will vary depending on the type of transplant (PK, DALK, DSEK, or DMEK) as described above. The surgery itself can take anywhere from 30 minutes to 2 hours or more.
- Post-operative Care: The Crucial Healing Phase:
- Eye Drops: You will be prescribed several types of eye drops (antibiotics to prevent infection, steroids to reduce inflammation and prevent rejection, and possibly others). Adhering strictly to the schedule and duration of these drops is critical for a successful outcome.
- Eye Shield/Patch: You will likely wear a protective eye shield, especially at night, for several weeks to prevent accidental rubbing or pressure on the eye.
- Positioning (for DSEK/DMEK): If you undergo DSEK or DMEK, you will be instructed to lie flat on your back for a significant portion of the first few days (e.g., 75% of the time for 3-5 days). This helps the air bubble (which holds the new graft in place) press against the cornea and ensure proper adhesion.
- Activity Restrictions: You will have restrictions on strenuous activities, heavy lifting, bending, rubbing your eye, and getting water directly into your eye for several weeks.
- Follow-up Appointments: Frequent follow-up visits with your ophthalmologist are essential in the initial weeks and months to monitor healing, check eye pressure, adjust eye drops, and address any concerns.
Recovery and What to Expect: A Journey to Clear Vision
The recovery process after Cornea Transplant Surgery is a journey, and patience is key. The timeline for visual recovery varies significantly depending on the type of procedure:
- DSEK/DMEK: Often, patients notice significant visual improvement within a few weeks to 2-3 months. The vision can continue to be refined over 6 months.
- DALK: Visual recovery is typically faster than PK but slower than endothelial transplants, often taking 3-6 months for good vision to emerge.
- PK: This has the longest visual recovery, often taking 6-12 months or even longer for vision to stabilize. This is because the sutures need to be removed gradually, and astigmatism can be a significant factor.
Potential Complications (and How They Are Managed):
While Cornea Transplant Surgery is highly successful, like any surgery, it carries potential risks. Your ophthalmologist will discuss these in detail:
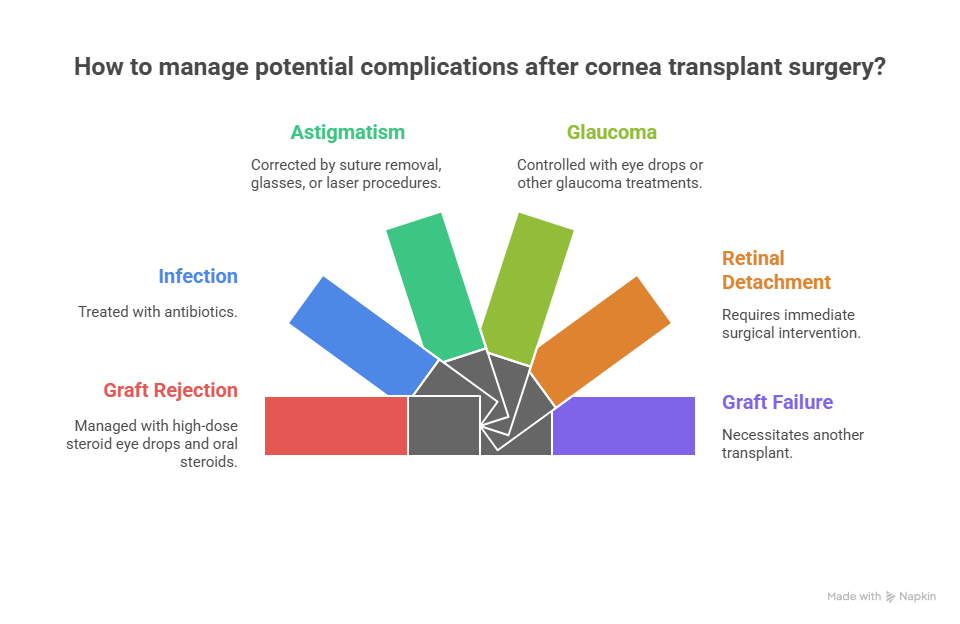
- Graft Rejection: This is the most common and serious complication, where the body’s immune system recognizes the donor tissue as foreign and tries to reject it. Symptoms include redness, pain, light sensitivity, and blurred vision (RSVP: Redness, Sensitivity, Vision decrease, Pain). Rejection can occur at any time, even years after surgery. It is managed with high-dose steroid eye drops and sometimes oral steroids. Early detection and aggressive treatment can often reverse rejection.
- Infection: Though rare due to antibiotics, a severe infection can occur.
- Astigmatism: Especially common after PK, where the irregular curvature created by the sutures can cause blurred vision. This is managed by selective suture removal, and sometimes by glasses, contact lenses, or further laser procedures.
- Glaucoma: Increased eye pressure can sometimes develop after a transplant, especially with long-term steroid use. This is monitored and managed with eye drops or other glaucoma treatments.
- Retinal Detachment: A rare but serious complication where the retina pulls away from the back of the eye.
- Graft Failure: The donor cornea may simply fail to remain clear over time, necessitating another transplant.
Need clarity about Cornea Transplant Surgery?
Don’t let corneal problems affect your vision. Our eye specialists provide advanced cornea transplant care with safe and effective procedures. Book your consultation today to restore clear vision.
Book Cornea ConsultationLiving with a Cornea Transplant: Lifelong Care
A successful Cornea Transplant Surgery can dramatically improve vision and quality of life. However, it requires a lifelong commitment to care:
- Regular Follow-up Appointments: These are crucial for monitoring the health of the transplanted cornea, checking for signs of rejection, managing eye pressure, and addressing any vision changes.
- Adherence to Eye Drop Regimen: You may need to use steroid eye drops (often at a lower dose) for many years, sometimes indefinitely, to prevent rejection.
- Eye Protection: Continue to wear protective eyewear during activities that could cause eye injury.
- Awareness of Rejection Symptoms: Know the RSVP symptoms (Redness, Sensitivity, Vision decrease, Pain) and contact your ophthalmologist immediately if they occur. Prompt action can save the graft.
Your Vision, Our Priority: Expert Care at Indira Gandhi Eye Hospitals
What is Cornea Transplant Surgery is a question that opens the door to renewed vision for many. It’s a testament to the advancements in ophthalmology and the profound generosity of eye donors. If you or a loved one is facing corneal disease and considering this life-changing procedure, choosing an experienced and dedicated team is paramount.
At Indira Gandhi Eye Hospitals, our specialized corneal surgeons possess extensive expertise in performing all types of Cornea Transplant Surgery and its procedures, including the most advanced lamellar techniques like DALK, DSEK, and DMEK. We utilize state-of-the-art diagnostic equipment and surgical technology to ensure precise, safe, and effective outcomes. Our comprehensive care extends beyond the operating room, providing meticulous pre-operative counseling and diligent post-operative management, ensuring you are supported at every step of your journey to clearer vision. We are committed to restoring your sight and enhancing your quality of life.
For a comprehensive evaluation, personalized advice on What is Cornea Transplant Surgery, or to explore your options, we invite you to connect with us. Visit our website at https://indiragandhiehospital.com/ to learn more and schedule an appointment. Let Indira Gandhi Eye Hospitals be your trusted partner in bringing the world back into clear focus.
Frequently Asked Questions (FAQs) About Cornea Transplant Surgery
How long does it take to recover full vision after Cornea Transplant Surgery?
The time to full visual recovery varies significantly depending on the type of Cornea Transplant Surgery. For full-thickness transplants (PK), it can take 6-12 months or even longer, while for partial-thickness endothelial transplants (DSEK/DMEK), significant improvement can often be seen within a few weeks to 2-3 months.
Where do donor corneas come from for Cornea Transplant Surgery?
Donor corneas come from deceased human donors who, or whose families, have generously consented to eye donation. The tissue is meticulously screened and tested by eye banks to ensure it is healthy and safe for transplantation.
What are the main risks of Cornea Transplant Surgery?
The main risks of Cornea Transplant Surgery include graft rejection (where the body’s immune system attacks the donor tissue), infection, astigmatism (especially after full-thickness transplants), and increased eye pressure (glaucoma). Your surgeon will discuss these risks in detail.
Will I need to take anti-rejection medication for my transplanted cornea?
Yes, you will typically need to use steroid eye drops for many months, often for years, and sometimes indefinitely, to help prevent graft rejection. The specific duration and dosage depend on the type of transplant and your response.
Can I get a second Cornea Transplant Surgery if the first one fails?
Yes, it is often possible to undergo a second or even third Cornea Transplant Surgery if a previous graft fails, although the success rates may be slightly lower with subsequent transplants. Your ophthalmologist will assess your case to determine the best course of action.
Is Cornea Transplant Surgery painful?
The Cornea Transplant Surgery itself is performed under anesthesia, so you will not feel pain during the procedure. After surgery, you may experience some mild to moderate discomfort, grittiness, or soreness, which can typically be managed with prescribed pain medication and eye drops